This page was originally posted on September 21, 2006. It has been the most viewed page on this blog. Updated February 22, 2013.
The other day a student asked me where the phrase “red flag” originated. He had also heard of yellow flags, and suspected that there were other colours of flags to indicate barriers to recovery. Well, we looked in various glossaries of medical and medical education terms, without success. So I e-mailed Dr. Shawn Thistle, and, sure enough, he helped. It is difficult to find where these terms originated (try Googling blue flags!) and Dr. Thistle thinks they may just be part of every doctor’s vocabulary. (Ever since I wrote the title above, I can’t get Dr. Seuss’s One fish two fish red fish blue fish out of my head.)
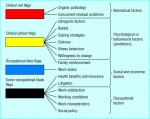
Red flags/clinical red flags (biomedical factors) ~
These help identify potentially serious conditions, and are often listed in practice guidelines. Here is a description from Chapter 13 of the Clinical guidelines for chiropractic practice in Canada [Glenerin Guidelines]:
The main focus for the prevention of complications is the recognition of well-known and established indicators or “red flag” signs and symptoms which may require careful assessment and reassessment, changes in treatment plan, or other appropriate action, such as emergency care or referral to another health care specialist. Ignoring these “red flag” indicators increases the likelihood of patient harm.
Yellow flags/clinical yellow flags (psychological or behavioural factors/predictors) ~
These indicate psychosocial barriers to recovery. Here is a definition from
New Zealand acute low back pain guide: incorporating the Guide to assessing psychosocial yellow flags in acute low back pain:
Yellow Flags are factors that increase the risk of developing or perpetuating long-term disability and work loss associated with low back pain … Before proceeding to assess Psychosocial Yellow Flags it is important to differentiate between acute, recurrent and chronic presentations. Evidence suggests that treating chronic back pain as if it were a new episode of acute back pain can result in perpetuation of disability.
Blue flags/occupational blue flags (social and economic factors) ~
These refer to conditions in the workplace that may inhibit recovery. Examples are monotony, low degree of control, poor relationships or high work demands.
Black flags/socio-occupational black flags (occupational factors) ~
These are also used for workplace issues, but refer to organizational issues such as financial reliance on disability benefits, workers’ compensation issues, or employer attitudes to the sick worker.
References:
Helliwell PS, Taylor WJ. Repetitive strain injury. Postgrad Med J 2004;80(946):438-43.See An Approach to Diagnosis
Main CJ, Williams AC. ABC of Psychological Medicine. Musculoskeletal pain. BMJ 2002;325(7363):534-7.
Click on the image below for The clinical flags approach to obstacles to recovery from back pain and aspects of assessment.
From: Main CJ, Williams AC. ABC of Psychological Medicine. Musculoskeletal pain. BMJ 2002 Sep 7;325(7363):534-7. PMC version
Filed under: Chiropractic/CAM, Patient Care | Comments Off on Red Flags, Yellow Flags, Blue Flags, Black Flags